As a new or experienced coach, you realize that approaching a person’s well-being from a holistic perspective yields better long-term results and honors the client more completely. This free training highlights what you will want to know and consider. Here’s how you can incorporate holism in your life and that of your client’s.
As a new or experienced coach, you realize that approaching a person’s well-being from a holistic perspective yields better long-term results and honors the client more completely. This free training highlights what you will want to know and consider. Here’s how you can incorporate holism in your life and that of your client’s.
Detoxification as Part of Holistic Health Protocol
As a coaching strategy, talking about detoxification or a cleansing diet might be one of your best tools. A recent trend reveals a surge of people who are fasting, cleansing, and detoxing. Why is this a potential coaching tool? Because it is a powerful nutritional strategy. Whether the cleanse comes from a water-only fast, juice fast, or an all-herbal cleanse, the potential for profound results is significant. Because we live in a toxic world, we must adapt to the times, and we have to get the body clean. One of the best ways to do that is through various fasting and cleansing programs.
Regardless of type, we can help our client detox faster. Again, this is where the Certified Holistic Nutrition Coach is vital to coaching a client holistically. Here’s how to improve client health naturally.
When you detox your mind, you detox your body
The mind and body exist on a continuum. There are so many traditional cultures and philosophies, religions, and great thinkers who have stated that the mind is a rarefied body, and the body is solidified mine. This is another way of saying that mind and body exist on a continuum -whereby if you impact one you impact the other. Many of our clients believe that they are going into a cleansing diet to get the poisons out of their bodies. This is only part of the equation, however. You see, we also have poisons in the mind; this is the negative self-talk (just one example) and useless dialogues we often have with ourselves, including:
“I’m no good”,
“I’m not enough”
“I’m not lovable”
“I need to look different”
“I need to make more money”
…and all the things that we say to ourselves when our minds are toxic with our thoughts. This conditional type of love we create only works to make us believe that we are not okay now, just as we are.
Consider for a moment fasting and cleansing – they are ancient strategies. Cultures and traditions from the past have a record of this in historical written works. When the prophets of older times went out into the wild to begin a fast or cleanse, did they do it to look good? Not really. Maybe instead it was done so they could have a vision, or they did it so they can get connected to the truth of who they were. Some sought to empower their life on a deeper level. The goal was to aim at cleaning out their system from the world, of the culture, of the thoughts, and of all the chatter that is often in our minds. It was a way to get rid of the mind pollution they disliked. It was a way to effectively get back to the business of what’s pure and real.
Loving one’s body in a toxic-free space
Our clients represent a diverse group. Not all are grounded and centered. For example, if your client spends time gossiping, if they speak ill of other people, if they’re constantly doing a type of self-sabotage type of attack, we need to coach them toward letting go. If holding grudges or hanging onto negativity in their mind and their heart, they begin to lose their light. We lose our energy and it’s easier for us to become toxified. When we know a client wants to go on a fast or a cleanse, we coach them to notice what wants to leave their life, they notice the old habits and old thoughts. They should notice the poisonous beliefs that need to be let go. When we coach our clients to clean their inner house the outer body cleans house as well. When we clean the body we also clean the mind, it is circular. This coaching action is seen as almost ethereal and is intended to get the CHNC excited to learn more about the breakthrough body of work in this area. You may have heard of mind-body fitness; now imagine mind-body nutrition. This is how we truly help clients to forever transform their relationship with food, their body, and their health.
Heart Disease and Holistic Alternatives
This section is mainly related to integrative strategies used to control and manage heart disease.
Emotional Resilience and Social Healing
Coronary artery disease is one of the few areas in which we have outcomes data on the actual application of an integrated and holistic approach. This has contributed to lifestyle recommendations that are now considered very mainstream and conventional. Typically, we would see these recommendations to include a lifestyle regimen featuring mediation, yoga, sound nutrition (often a low- fat vegetarian diet), smoking cessation, regular exercise, and community support. These options have shown results that not only stop the progression of CAD but reverses it.
Social support, believed to be the core of our connections with others, is critical. The following are ways we coach clients to acquire this need:
- Becoming aware of what you say and how you say it
- Finding a group that supports you
- Understanding confession, redemption, and forgiveness
- Working to be more compassionate, altruistic, and of service to others
Using psychotherapy - Making commitments to others
- Meditating
- Making commitments to others
- Meditating
Mind/Body Practices and Stress Reduction
The use of mind/body practices lowers the excitation level of the body, which has positive impacts on blood pressure, cholesterol levels, sugar metabolism (and therefore diabetes), mood state, sleeping patterns, and communication abilities. Their use is recommended by the American College of Cardiology.
Mind-body practices include meditation, guided imagery, stress reduction, and biofeedback. Often, these are referred to as Bodyways.
Several research institutes have done extensive research into the overall benefits (including cardiac), of mind/body practices, this data has become an interesting resource for educational materials used in coaching, research findings, and tools for relaxation practices.
While there are extensive resources available for learning and practicing such techniques on one’s own, instruction from a teacher or practitioner is helpful, and practice with others is very supportive. Wherever you live, it is likely you can find local resources through colleges and schools, community centers, churches, and health clubs. Because some of these practices are things you learn to do for yourself, long-term financial impacts are minimal. Once proficient with a Bodyway, you may even feel compelled to try it on your clients (where appropriate).
Botanicals and Supplements
Ideally, nutritional substances are optimally obtained through the food we eat. However, some supplemental substances are of some benefit for those with CAD. Typical doses for each botanical are indicated below. However, your client is always advised to talk with their healthcare provider before adding botanicals to a holistic health regimen. It is also important to ask about the right dosage amount.
Omega-3 supplements: fish oil supplements (<3 g/day), flaxseed oil (1 Tbsp daily) or up to 3 Tbsp/day finely ground flaxseed
Soluble fiber: psyllium (10-25 g/day)
Garlic, raw or lightly cooked to preserve the bioactive components (1-2 cloves daily)
Recommended dietary intake of magnesium (men – 420 mg/day; women – 320 mg/day)
Folic acid supplementation, 0.4-1mg/day (plus vitamins B6, 25mgs, and B12 0.5mg)
Hawthorne (600-1,800 mg/day); it must be used with caution if digoxin is also prescribed
Carnitine (1-3 mg/day) and Coenzyme-Q10 (100-200mg/day)
How to use Integrative Therapies in Your Heart Disease Care
Individuals with coronary artery disease are generally on prescription medications to protect the heart. Changing or stopping that medication can be potentially life-threatening. If individuals with CAD pursue complementary therapies, such as homeopathy, Traditional Chinese Medicine, or naturopathy, their providers must consider potential drug interactions between cardiac medications and any natural products (for example, Chinese herbs).
Holistic Brain Health
We have struggled at times to make good use of the ongoing research in our quest to understand the root causes and progression of Alzheimer’s and the factors that may protect the brain from this devastating illness.
Alzheimer’s Disease (AD) is the most common form of dementia, affecting a person’s memory, thinking, and behavior to the point where they don’t recognize themselves and their loved ones. Approximately 5.5 million people age 65 and older have Alzheimer’s Disease. Nearly 200,000 people under age 65 have “younger-onset” AD. Symptoms start slowly and worsen over time, ultimately interfering with independent living and quality of life.
This is why we developed the Certified Sleep Science Coach Certification for you.
Signs to look for include:
- Persistent forgetting of recently learned information and important dates or events
- Difficulty planning, problem-solving, completing familiar tasks, and understanding time
- Difficulty processing visual images, object distance and contrast
- Trouble maintaining a conversation
- Social withdrawal and depression
- Changes in mood and personality, usually becoming anxious, suspicious, or confused
Scientists believe the disease process begins when protein deposits build up in the brain tissue and damage nerve cells. This can evolve over 10-20 years before symptoms are noticed. While family history can increase your risk, many factors influence the onset and progression of AD. Maintaining a healthy lifestyle, as outlined below, can help alter your brain’s destiny.
The Brain-Body Health Connection. Several illnesses are linked to an increased risk for AD, including heart disease, stroke, high blood pressure, and diabetes. To protect your mind from cognitive decline, exercise daily, eat more whole foods, learn new skills, meditate, read regularly, and get quality sleep each night.
Smart food choices to fight aging. Choosing fresh, nutrient-rich foods is vital for brain health (and the body, too). Select organic foods to decrease exposure to toxins that exist in conventional farming. Limit your intake of caffeine, sugar, alcohol, refined grains, and packaged foods to ensure optimal health benefits from your food.
Help clients manage Stress. Stress elevates hormones in the body that increase inflammation which, over time, interferes with optimal functioning and contributes to illness. Relax with yoga, mindful walking, or guided imagery to help keep these hormones in balance.
Sleep as needed. We need just as much sleep in our elder years as in our 30s and 40s. What does change is the brain’s ability to maintain continuity and quality of sleep, particularly deep sleep? Maintaining healthy sleep habits throughout your adult life can make it easier to maintain sleep quality as you age.
A personalized plan that meets your client’s unique needs. With any chronic condition, prevention is ideal. Once signs of cognitive decline are noticed, your client should seek expert guidance. At this time, we know one thing, however: more long-term studies are needed. But initial research shows that a personalized approach that incorporates natural medicines with lifestyle change can reverse cognitive decline for some people. For expert guidance in developing a personalized prevention or early intervention program, consult with a specialist in natural medicine treatments for Alzheimer’s Disease such as a Naturopathic Doctor or Functional Medicine practitioner.
Holistic Coaching Clients with Cancer
One thing we must be very clear about here: the CHNC does NOT diagnose or treat a client with any known illness unless they have a medical degree or an ND.
Many people who manage cancer are interested in trying anything that may help them, including complementary and alternative cancer treatments. Cancer can make us feel as if we have little control over our health, alternative cancer treatments may offer some feeling of control. But many alternative cancer treatments are unapproved, and some may even be dangerous.
To help you sort out the good from the bad, here are 10 alternative cancer treatments that are generally considered to be safe. There is growing evidence that these 10 alternative cancer treatments may provide some benefit.
How can alternative medicine help people with cancer?
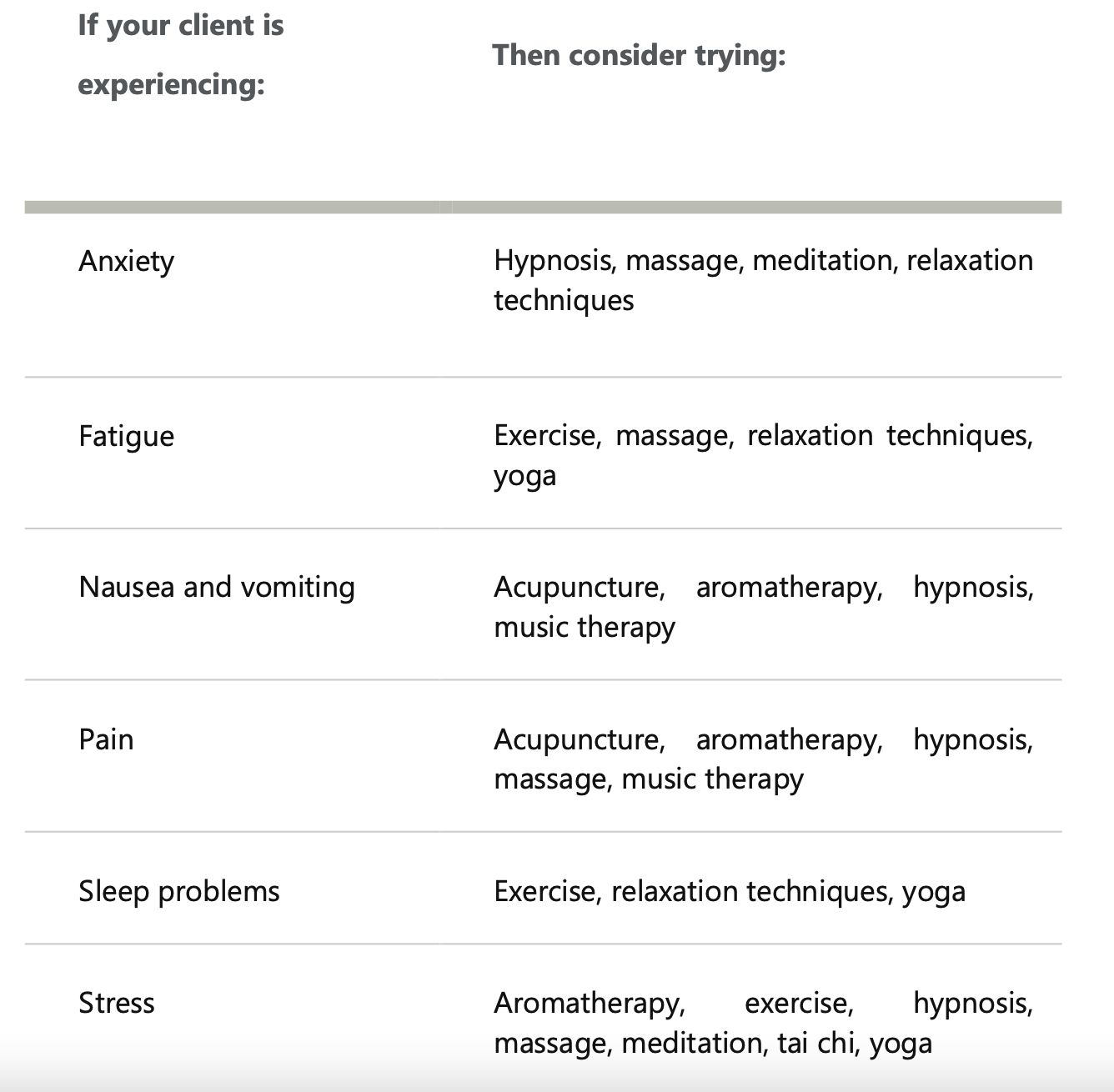
Alternative cancer treatments may not play a direct role in curing your cancer, but they may help patients cope with signs and symptoms caused by cancer and cancer treatments. Common signs and symptoms such as anxiety, fatigue, nausea and vomiting, pain, difficulty sleeping, and stress may be lessened by alternative treatments.
Integrating the best of evidence-based complementary and alternative cancer treatments with the treatments received from a doctor may help relieve many of the symptoms associated with cancer and its treatment. Discuss options with your client and together you can determine which strategies might work for them in support of their treatment, and which are likely to have no benefit.
Work closely with your doctor to determine the right balance between traditional medicines and alternative cancer treatments. While complementary and alternative cancer treatments, such as acupuncture, may reduce nausea or pain, they generally aren’t powerful enough to replace cancer medications from your doctor.
Holistic Alternatives to Help Clients Managing a Cancer Diagnosis
These alternative cancer treatments have shown some promise in helping people with cancer. Again, we caution all CHNC’s to exercise extreme caution when working with a client who is being treated by a physician.
Acupuncture
During an acupuncture treatment, a practitioner inserts tiny needles into your skin at precise points. Studies show acupuncture may help relieve nausea caused by chemotherapy. Acupuncture may also help relieve certain types of pain in people with cancer.
Acupuncture is safe if it’s performed by a licensed practitioner using sterile needles. Ask your doctor for names of trusted practitioners. Acupuncture isn’t safe if you’re taking blood thinners or if your client has low blood counts for some markers, so always defer to a medical professional before recommending this as a strategy.
Aromatherapy
Aromatherapy uses fragrant oils to provide a calming sensation. Oils, infused with scents such as lavender, can be applied to your skin during a massage, or the oils can be added to bathwater. Fragrant oils can also be heated to release their scents into the air. Aromatherapy may help relieve nausea, pain, and stress.
Aromatherapy can be performed by a practitioner and is generally safe, though oils applied to your skin can cause allergic reactions. People with cancer that is estrogen-sensitive, such as some breast cancers, should avoid applying large amounts of lavender oil and tea tree oil to the skin.
Exercise
Exercise may help to manage signs and symptoms during and after cancer treatment. Gentle exercise may help relieve fatigue and stress and help support better sleep. Many studies now show that an exercise program may help people with cancer live longer and improve their overall quality of life.
If your client hasn’t already been exercising regularly, be sure that they check with their doctor before beginning an exercise program. Start slowly, adding more exercise over time. Aim to work up to at least 30 minutes of exercise most days of the week. You can help by becoming a NESTA Certified Personal Fitness Trainer.
Hypnosis
Hypnosis is a deep state of concentration. During a hypnotherapy session, a therapist may use a gentle voice and helping the client relax. The therapist will then help gain focus on goals, such as controlling pain and reducing stress.
Hypnosis may be helpful for people with cancer who are experiencing anxiety, pain, and stress. It may also help prevent anticipatory nausea and vomiting that can occur if chemotherapy has created harsh side-effects previously. When performed by a certified therapist, hypnosis is safe. But the therapist should know if your client is managing a history of mental illness.
Massage
During a massage, the practitioner kneads the skin, muscles, and tendons to relieve muscle tension and stress and promote relaxation. Several massage methods exist. Massage can be light and gentle, or it can be deep with more pressure.
Studies have found massage can help relieve pain in people with cancer. It may also help relieve anxiety, fatigue, and stress.
Massage can be safe when done by a knowledgeable massage therapist. Many cancer centers have massage therapists on staff, or a doctor can refer clients to a massage therapist who regularly works with people who have cancer.
Meditation
Meditation is a state of deep concentration when we focus our mind on one image, sound, or idea, such as a positive thought. When meditating, try to do deep-breathing or relaxation exercises. Meditation may help people with cancer by relieving anxiety and stress.
Meditation is generally safe. Clients can meditate on their own for a few minutes once or twice a day or take a class with an instructor.
Music therapy
During music therapy sessions, clients might listen to music, play instruments, sing songs, or write lyrics. A trained music therapist may work through activities designed to meet your client’s specific needs, or they may prefer to participate in music therapy in a group setting. Music therapy may help relieve pain and control nausea and vomiting.
Music therapy is safe and doesn’t require any musical talent to participate. Many medical centers have certified music therapists on staff.
Relaxation techniques
Relaxation techniques are ways of focusing your attention on calming your mind and relaxing your muscles. Relaxation techniques might include activities such as visualization exercises or progressive muscle relaxation.
Relaxation techniques may help relieve anxiety and fatigue. They may also help people with cancer sleep better.
Relaxation techniques are safe. Typically, a therapist leads the client through calming exercises, and eventually, clients may be able to do them on their own or with the help of guided relaxation recordings.
Tai chi
Tai chi is a form of exercise that incorporates gentle movements and deep breathing. Tai chi can be led by an instructor, or clients can learn tai chi on their own, following books or videos. Practicing tai chi may help relieve stress.
Tai chi is generally safe. The slow movements of tai chi don’t require great physical strength, and the exercises can be easily adapted to your abilities. Still, consulting a doctor before beginning tai chi is recommended. Don’t do any tai chi moves that cause pain.
Yoga
Yoga combines stretching exercises with deep breathing. During a yoga session, the client will position their body in various poses that require bending, twisting, and stretching. There are many types of yoga, each with its own variations. Yoga may provide some stress relief for people with cancer. Yoga has also been shown to improve sleep and reduce fatigue.
Before beginning a yoga class, ask your doctor to recommend an instructor who regularly works with people with health concerns, such as cancer. Avoid yoga poses that cause pain. A good instructor can instruct on the use of alternative poses that are safe for your client.
You may find some alternative treatments work well together. For instance, deep breathing during a massage may provide further stress relief. You can earn your credential as a yoga instructor from NESTA.
Cancers of the Digestive System
Stomach cancer or gastric cancer usually starts in the inner lining of the stomach where cancer cells grow into a tumor. Symptoms and treatment options for gastric cancer may vary depending on where it begins. Commonly, stomach cancer begins in the mucosa, which is the innermost layer of the stomach that generates stomach acid and digestive enzymes.
Stomach cancer develops at a gradual pace for many years. It can metastasize to other parts of the body and can spread to other organs and lymph nodes.
It’s important to note that stomach cancer is not synonymous with other cancer types that form in the different organs in the abdomen such as the colon, liver, pancreas, or small intestine.
Current estimates show that there will be roughly 28,000 new cases of stomach cancer in 2020 and nearly 12,000 of these cases are expected to die from this condition.
The structure of the stomach
The stomach is a musculo-membranous structure joined by the esophagus and the duodenum or small intestines. The stomach is shaped like the letter J and it serves as a food reservoir and an initiator of the digestive process. The food is held in the stomach temporarily until the stomach lining secretes digestive juices that juices which act on the food to break it down chemically. This article shows the step-by-step process of digestion.
Stomach carcinomas can be grouped according to the total appearance:
- Protruding
- Penetrating
- Spreading
The different types of stomach cancer are:
- Adenocarcinoma – a type of gastric cancer that develops in the mucosa and accounts for 95% of stomach cancer.
- Lymphoma – a type of stomach cancer that begins in the lymph nodes on the stomach wall and accounts for about 4% of cases
- Gastrointestinal Stromal Tumor – a type of gastric cancer that forms in the interstitial cells of the stomach wall. Some of them may turn out benign.
- Other rare types – Rarer forms of stomach cancer are squamous cell carcinoma, small cell carcinoma, and leiomyosarcoma
Stomach cancer was once the top cause of cancer-related deaths, but the mortality rate of this cancer type has decreased nearly 100 years ago. Possible reasons that contributed to the fewer incidences of gastric cancer are the advent of food refrigeration and the increased use of antibiotics.
Symptoms indicative of the disease such as:
While stomach cancer doesn’t usually manifest symptoms during its early stages, it still pays to be aware of the signs and symptoms that can be
● Unexplained weight loss
● Pain in the abdomen
● Indigestion
● Nausea
● Vomiting
● Anemia
● Appetite Loss
● Discomfort in the abdomen, typically above the navel
● Feeling full after eating only a small amount of food
● Swelling in the abdomen
● Difficulty swallowing
● Jaundice or the yellowing of the skin and eyes
● Constipation and diarrhea & Blood in the stool or dark bowel movement
It’s important to note that some of the symptoms listed can indicate another health condition. To be completely sure about what these signs signify, have your client seek medical attention as soon as they notice anything unusual with their body. Early detection is vital, and in this way, problems can be detected early on and receive appropriate treatment.
Risk Factors
The average risk for stomach cancer in a person’s lifetime is 1 in 11. The factors that can influence a person’s chances of incurring the disease are the following:
Age – Older people are at more risk than younger individuals. Most cases are diagnosed among people who are between the ages of 60 and 80.
Infection and Viruses – H. Pylori bacteria can trigger stomach cancer as it can cause inflammation and pave way for precancerous changes in the stomach. People with the condition are found to have a higher rate of H. Pylori in their stomachs. Also, H. Pylori can lead to stomach lymphoma called MALT (mucosa-associated lymphoid tissue lymphoma), which also increases the risk of stomach cancer. Being exposed to the Epstein Barr virus also increases this risk.
Diet – A diet high in smoked and processed food, salted meat, and pickled vegetables can increase your chances of having stomach cancer.
Medical conditions – Health problems such as hypertrophic gastropathy, pernicious anemia, inherited cancer syndromes, and common variable immune deficiency can make some clients more prone to developing stomach cancer.
Occupation – Those who work in coal, metal, and rubber industries, are more at risk for stomach cancer.
Family history – Those with a first-degree relative—a parent, sibling, or child— also have a higher likelihood of being diagnosed with the disease.
Blood type – People who have Type A blood are more likely to develop the condition, but the exact reason is still unclear and being researched.
Stomach polyps– Growths in the stomach increases your chances of developing gastric cancer Obesity or being overweight – Excessive weight is a suspected cause of stomach cancer. Its link or relationship with the disease still needs to be examined and researched.
Tobacco use – Smokers have twice the risk of stomach cancer as opposed to those who don’t use tobacco.
Prevention
Just like with other cancers, preventing stomach cancer has a lot to do with minimizing the risk factors we can control. Here are some of the ways.
Maintain a healthy diet – A diet rich in smoked and salty foods are said to increase stomach cancer risk. Steer clear of those food items and increase your portions of fruits and vegetables every day. These food items have fiber and nutritious content that can help lessen your stomach cancer risk and aid in maintaining an ideal weight.
Treat stomach infections – When not addressed, infections can increase the chances of developing stomach cancer. That’s why they need to be treated right away, to eliminate the risk of problems down the road.
Avoid smoking – Smoking doubles a person’s risk of gastric cancer. Clients who smoke should quit to lower the risk of stomach cancer; recommend cessation efforts when appropriate (without issuing directives or warnings).
Methods of Detection Gastric Cancer
There are several ways and procedures to detect stomach cancers in the body, these are:
Physical examination and medical history – During the consultation, clients are typically asked questions about symptoms, risk factors, family history of stomach cancer, and other information about general health. If the initial assessment somehow indicates cancer, your client may then be referred to a specialist or recommended to undergo tests.
Upper endoscopy – A procedure wherein an endoscope is passed down the person’s throat to see the esophagus, stomach, and parts of the small intestine.
Endoscopic ultrasound – A procedure that uses sound waves to produce an image of the stomach.
Biopsy – A procedure done to collect samples from the stomach and its other parts to determine whether cancer is present or not. This can be done during endoscopy.
Upper gastrointestinal series – In this test, the person will drink a chalky solution that contains barium. This will coat the lining of the esophagus, stomach, and small intestine so that they will show up more clearly on the X-ray.
CT Scan – An imaging test that generates intricate and detailed pictures of the body’s interior.
MRI Scan – This imaging test is less commonly used to detect stomach cancer, but it can also create a clear visualization of what’s happening inside the body. It takes longer than CT scans.
PET Scan – A procedure that detects cancer spread and location with the help of a radioactive substance injected in the veins.
Chest X-Ray – An imaging test that helps detect cancer that has spread to the lungs.
Laparoscopy – A procedure usually done when cancer is already diagnosed. It is conducted to detect tumors that were possibly missed by other imaging tests. It can also be recommended before a surgical procedure to make sure of the position of the cancer and to determine whether surgery is still the right course of action to remove cancer completely.
Laboratory Test – Different kinds of laboratory exams can be prescribed to detect signs of stomach cancer. These include CBC to detect anemia and fecal occult blood test to detect any traces of blood in the stool that can be invisible in plain sight.
You have many career training options as a next step. Click here to explore them all >>>